Republicans Are Playing With Fire – and Seniors’ Earned Benefits – By Risking Default

Thursday’s breaching of the debt ceiling by the U.S. government is making seniors’ advocates very nervous. The federal government is now on track to default on its financial obligations (including the ability to make Social Security and Medicare payments) as early as June — unless Congress lifts the debt ceiling, which House Republicans refuse to do without spending cuts. NCPSSM legislative director Dan Adcock told CNBC that the country is heading for a fiscal “train wreck” if the GOP maintains its hardline position.
Raising the debt ceiling is supposed to be a routine matter of business so that the government can meet its existing financial obligations. In fact, Congress has raised the debt ceiling 78 times since 1960. If the debt ceiling is not adjusted before the Treasury Dept. exhausts “extraordinary measures” to pay the federal government’s bills, the U.S. will default on its debts, which would induce severe economic turmoil. Nonetheless, House Republicans are refusing to raise the debt ceiling unless Democrats agree to cut crucial programs. As CNN’s Jake Tapper put it, “Republicans are vowing to cut future spending before agreeing to pay bills that are already due.”
NCPSSM’s President and CEO, Max Richtman, warns that a federal default would not only invite economic catastrophe, but could negatively impact older Americans:
“Congressional Republicans are playing with fire by risking a government default on its financial obligations — an outcome that is more likely today as the U.S. reached its legal borrowing limit. A default would hit the nation’s seniors especially hard, as the payment of Social Security, Medicare, and Medicaid benefits would be jeopardized.” – Max Richtman, 1/19/23
Without the legal authority to borrow beyond the current debt ceiling, Social Security, Medicare, Medicaid, and other payments may not be made on time and in full unless Congress approves an increase in the debt limit. Even a short delay in the payment of Social Security benefits would be a burden for the millions of Americans who rely on their earned benefits to pay for out-of-pocket health care expenses, food, rent and utilities.
Republicans have threatened to use the debt ceiling crisis to extract concessions on spending from Democrats and the White House. Seniors’ advocates became especially concerned when key GOP members seemed to suggest that this crisis presented an opportunity to force changes to ‘entitlements.’
President Biden has vowed to veto any legislation that would cut Social Security, Medicaid, and other vital social safety net programs. Today, the White House announced that the President would not negotiate with Congressional Republicans about the debt ceiling. Senate Republican Leader Mitch McConnell told CNN today that negotiations are inevitable, but that “America has never defaulted on its debt and never will.”
While cooler heads may prevail in the Senate, the ultra-MAGA faction of the House GOP caucus has insisted that there cannot be a ‘clean’ lifting of the debt ceiling without pre-conditions. In order to become House Speaker, Kevin McCarthy agreed to demands by right-wing Republicans that raising debt ceiling must be tied to spending cuts.
“If the House GOP refuses to raise the debt limit and replaces responsible governance with fiscal extortion, our most vulnerable citizens will pay the price. This is definitely not what the American people voted for last fall.” – Max Richtman, 1/19/23
In 2011, Tea Party Republicans pushed the country to the brink of a default in an attempt to force spending cuts. Democrats stood firm against the GOP’s demands, but the outcome of that debt battle included GOP-imposed spending caps which hobble Congress to this day — and the downgrading of the United States’ credit rating around the world. Senator Chris Coons (D-CT) said Thursday afternoon, “I was here 12 years ago and it didn’t work out for (Republicans) then, and I don’t think it will work out for them now.”
McCarthy Speakership Battle May Cost Seniors in the Long Run



Kevin McCarthy’s battle for the House speakership made for compelling political theater this week, but it could have dramatic implications for America’s seniors. According to news reports, McCarthy (R-CA) made concessions to holdout House members that would empower right-wingers in Congress who want to slash Social Security and Medicare — in order to fulfill his personal ambition to become Speaker.
CNN’s Manu Raju reported Friday afternoon that McCarthy agreed to demands from Freedom Caucus members regarding upcoming debt ceiling negotiations. In the putative deal, McCarthy reportedly has pledged not to raise the debt ceiling (so that the federal government can pay its existing obligations) without concessions on spending from Democrats and the White House on domestic programs.
If this reporting is accurate, it means that McCarthy has effectively agreed to risk a U.S. government default on its financial obligations (and the financial chaos that would ensue) in order to force cuts to Social Security, Medicare, and other safety net programs — despite the fact that these programs are incredibly popular and vital to the well-being of American seniors. (Not to mention that lifting the debt ceiling is essential for the U.S. to pay its existing bills.)
This scorched-earth strategy, which one CNN analyst characterized as “taking us to the brink of destruction,” is not what voters demanded in the 2022 elections. In fact, in denying Republicans an anticipated “Red Wave” last fall, the electorate clearly rejected MAGA extremism and MAGA-nomics.
Nevertheless, a small cadre of right-wing Freedom Caucus members are the ‘tail wagging the dog’ in McCarthy’s bid for the speakership. These extremists oppose spending on social programs no matter how important or popular those may be. (One commentator rightly branded them as “nihilists” who don’t believe in a functional federal government.)
We have seen this before. In 2011, Tea Party members instigated a battle over the debt ceiling that resulted in harmful caps on domestic spending that haunt us to this day. “I was around in 2011,” said former Obama advisor David Axelrod on CNN today, “and I remember that Republicans took us to the precipice of what would have been a catastrophe,” by risking a federal default on its financial obligations.
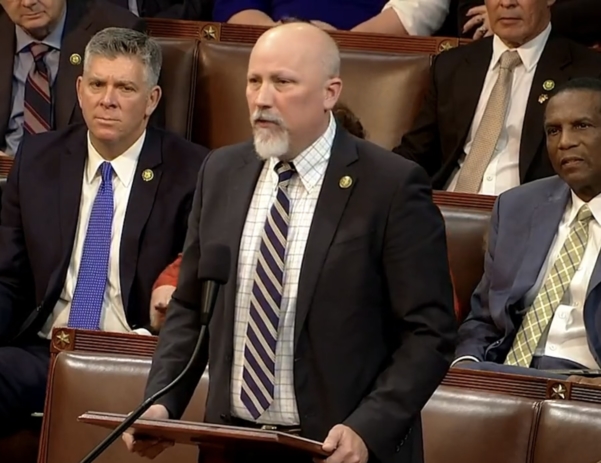
Rep. Chip Roy (R-TX) helped negotiate concessions from Kevin McCarthy
Beyond the debt ceiling maneuverings, Freedom Caucus members reportedly are wringing other concessions from McCarthy in return for their votes that also could be devastating for older Americans. These include rule changes that could make it harder to raise revenue and easier to cut spending on social programs.
The hard right would get approval power over some plum committee assignments, including a third of the members on the influential Rules Committee, which controls what legislation reaches the floor and in what form. And spending bills would have to be considered under so-called open rules, allowing any member to put to a vote an unlimited number of changes that could gut or scuttle the legislation altogether. – New York Times, 1/6/23
“That does not bode well for programs like Social Security and Medicare that are going to need an infusion of revenue,” says Maria Freese, policy advisor here at NCPSSM. “The new rules would make it easier for House Republicans to keep cutting taxes for the wealthy while gutting programs that everyday Americans depend on.”
If Kevin McCarthy does prevail (which as of Friday afternoon looks increasingly likely) and achieves his years-long dream of being House Speaker, seniors will be among those everyday Americans paying the price.
Does New Hill Spending Deal Affect Social Security & Medicare?
Congressional negotiators have avoided a government shutdown by reaching a compromise agreement on federal spending for the remainder of FY 2023. The Hill newspaper reported that lawmakers had “reached a bipartisan, bicameral framework that should allow them to finish an omnibus appropriations bill that can pass the House and Senate and be signed into law by the President.’” We spoke to NCPSSM legislative director Dan Adcock about the spending deal and whether it impacts Social Security and Medicare.
Q: What basically happened here?
Adcock: Republicans and Democrats were able to forestall a government shutdown that would have been triggered on Friday had they failed to agree on spending for the remainder of FY 2023. Late yesterday the two parties arrived at a compromise agreement on appropriations for the rest of the fiscal year, which began on October 1, 2022. The result will be an “Omnibus” spending bill because it combines all congressional appropriations into a single piece of legislation.
Q: Does this process affect Social Security and Medicare benefits?
Adcock: Not directly. Social Security and Medicare are considered “mandatory spending,” and are funded according to the laws that created them. They are not part of the annual appropriations process. What Congress is wrangling over now is called “discretionary spending,” which goes toward the day to day operation of the federal government. On the other hand, if there had been a government shutdown, Social Security Administration customer service could have been disrupted.
Q: What about funding for the Social Security Administration?
Adcock: Funding for SSA is, indeed, part of the annual appropriations process. We have urged Congress to appropriate $14.8 billion for Fiscal Year 2023, which is the level that President Biden requested in his budget. SSA badly needs these funds in order to improve customer service after more than a decade of budget cuts – and to work through the huge backlog in disability claims that built up during the pandemic.
Q: The current process is different than the debt ceiling negotiations, right?
Adcock: Yes. This week’s negotiations were about agreeing on appropriations to fund the daily operations of the government and avoid a shutdown. The debt ceiling issue is separate. Sometime during 2023 (most likely during the 3rd quarter), the federal government will have exhausted its ability to borrow money to meet its financial obligations — unless Congress raises or suspends the debt ceiling. Republicans, who will have a majority in the House in the 118th Congress, have threatened to use next year’s debt ceiling negotiations to extract cuts to Social Security and Medicare. Democrats will have to stand firm in the face of GOP pressure and refuse to consider cuts to Americans’ earned benefits.
Q: Is the spending agreement a done deal?
Adcock: The two parties have reached a tentative agreement on top-line numbers, but they still must determine the line item amounts for each federal agency and program in the actual spending bill. There’s also a lot of backroom work that goes into assembling a thousand-plus page bill like this. The congressional leadership are incentivized to finish by the end of next week so that they can head home for the holidays.
NCPSSM President Busts Social Security Myths at Sen. Harkin’s Forum



Some of the nation’s leading Social Security experts gathered in Des Moines, IA on Wednesday to discuss the future of a program buffeted by serious financial and political challenges. The forum, Roadmaps to Retirement, was presented by the Harkin Institute at Drake University and moderated by former U.S. Senator Tom Harkin (who also chairs the National Committee to Preserve Social Security and Medicare Advisory Board). NCPSSM President and CEO Max Richtman was among the experts on the panel, which also included Acting SSA Commissioner Kilolo Kijakazi and Assistant U.S. Labor Secretary Taryn Williams, among others.
During the forum, Senator Harkin asked Richtman to debunk several harmful myths which have undermined public perceptions of Social Security over the years – with many of these falsehoods perpetuated by conservative ideologues who have opposed the program from the beginning. Richtman told the audience that one of the most pernicious myths is that Social Security is “bankrupt” or “going broke”:
“While it’s true that the Social Security trust fund will become depleted in 2035 if Congress takes no preventative action, the program is not going bankrupt. Payroll taxes from workers will continue to cover 80% of benefits even if the trust fund is allowed to run dry. The only way Social Security could go “bankrupt” is if we had 100% unemployment and no one was working or paying into the program, which is unlikely to ever happen.” – Max Richtman, 12/7/22
Richtman also debunked the myth that the Social Security trust fund isn’t real — or that it consists of “worthless IOUs.” He explained that the $2.852 trillion in the trust fund is held in special interest-bearing Treasury bonds backed by “the full faith and credit of the United States of America.” He also pushed back on the notion that the government has been “stealing from Social Security” to pay for other expenses, a widespread belief which is patently untrue.
“Unfortunately, some of these myths have taken hold in the public’s mind. Many younger adults have bought into them and are cynical about the future of Social Security. Some young people believe that they are more likely to see Bigfoot or a U.F.O. than a Social Security check when they retire.” – Max Richtman, 12/7/22
Senator Harkin pointed out that, contrary to many younger adults’ perceptions, Social Security not only will be there for them when they retire, but the program provides insurance against disability and the loss of a family breadwinner to millions of young adults right now. In fact, workers have life insurance protection from Social Security worth over $725,000. Meanwhile, for a young disabled worker with a spouse and two children, the disability coverage they get through Social Security Disability Insurance (SSDI) is valued at over $580,000.
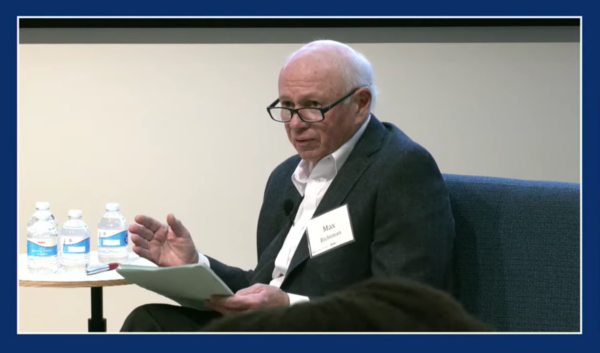
NCPSSM President Max Richtman: “The only way Social Security could go “bankrupt” is if we had 100% unemployment.”
Richtman and Senator Harkin agreed that more outreach to younger adults about Social Security is needed in order to maintain support for the program moving forward. “Hopefully there will be more education for young people as to how it works,” said Harkin. But the genesis of the forum was the Harkin Institute’s concern about financial security for current as well as future retirees. Experts have noted that the ‘three-legged stool’ of retirement security (retirement savings, employer provided pensions, and Social Security) is no longer strong enough for many workers to retire securely — mainly because it’s harder for working people to save for retirement and employers have largely stopped offering pensions.
This new reality, says Harkin, makes it even more important to preserve and strengthen Social Security, noting that 40% of Americans aged 65 and over rely on the program for at least half of their total income. Social Security Acting Commissioner Kijakazi pointed out that even higher percentages of women and communities of color depend on Social Security as their main income source. “Social Security was supposed to be a ‘floor’ for retirement income. But it was never intended to be the sole source of retirement income,” says Kijakazi.
Acting Social Security Commissioner Kilolo Kijakazi
Harkin and Richtman called on Congress to strengthen the program and expand benefits to reflect the realities of retiring in America in the 20th century. They both favor adjusting the payroll wage cap (which will be about $160,000 in 2023) so that high earners begin paying their fair share into the system. This measure, which is included in Rep. John Larson’s Social Security 2100 act, would boost the solvency of the trust fund beyond the 2035 depletion date. These proposals are overwhelmingly popular among the public. Senator Harkin cited a survey by the National Academy of Social Insurance (NASI), indicating that 83% of Americans agree it is critical to preserve Social Security benefits for future generations, even if it means increasing taxes paid by wealthier earners.
Acting Commissioner Kijakazi called on lawmakers to shore up Social Security sooner than later. “Congress does need to act to ensure we will be able to pay all benefits beyond 2035,” she said. “And we believe congress will act to take the steps needed to maintain the long-term solvency of the program.”
The Warnock-Walker Runoff Isn’t Just About the Size of the Democrats’ Senate Majority



(photo from www.warnockforgeorgia.com)
While it’s true that a runoff win by Senator Raphael Warnock would give the Democrats a 51-50 majority, there is more at stake for voters – especially seniors. They need Senator Warnock to remain in the Senate to fight for their vital Social Security and Medicare benefits – and to continue advocating for lower prescription drug prices. That’s why the National Committee to Preserve Social Security and Medicare has endorsed Rev. Warnock for re-election as a “champion for seniors.”
He proved this during his first two years in office. Senator Warnock introduced legislation to cap seniors’ out-of-pocket drugs costs at $2,000 per year and limit insulin costs to $35 a month. Both provisions became part of the Inflation Reduction Act, which became law in late summer. He has been a fierce advocate for expanding Medicaid in Georgia, one of the holdout states that has refused to implement coverage for lower-income workers. Expanding Medicaid improves health outcomes for everyone – especially communities of color.
Mindful of the need to boost seniors’ benefits and put Social Security on a sound financial path, Senator Warnock cosponsored the Social Security Expansion Act. During the fall campaign, he pledged to fight GOP efforts to privatize seniors’ earned benefits. Senator Warnock is – and will continue to be – a key defender of Social Security and Medicare.
Perhaps at no other time since the Great Depression have seniors’ earned benefits been so crucial. The pandemic took a heavy toll on seniors – both physically and financially. Before and during this crisis, Social Security and Medicare have functioned as social insurance lifelines, which is, of course, their original purpose.
Without Social Security, the poverty rate in Georgia would be a whopping 44%. For Black and Latino seniors – who are especially reliant on Social Security for income – the poverty rate would approach or exceed 50% without their earned benefits.
Despite the crucial role that Medicare and Social Security play in seniors’ lives, Republicans insist that both programs must be “reformed” – which really means cut and privatized. High-profile members of Herschel Walker’s party, including Sen. Rick Scott (R-FL) and Sen. Ron Johnson (R-WI) have proposed subjecting seniors’ earned benefits to an up or down vote every five years and placing both programs at the mercy of annual budget battles. Herschel Walker campaigned with Sen. Scott in October and would be a rubber stamp for any GOP plans to undermine Social Security and Medicare.



Sen. Rick Scott (L) and Herschel Walker (R)
Republicans have been crystal clear about their intentions. The House Republican Study Committee’s 2022 budget blueprint called for raising the retirement age to 70 (a huge benefit cut), reducing COLAs, and cutting benefits for “high earners,” an odd characterization since the cuts eventually could extend to workers earning $40,000 per year.
Seniors have suffered enough during the pandemic and post-pandemic economy. With inflation running over 7% this year and health care costs soaring, they depend on their Social Security and Medicare benefits now more than ever. Older Georgians need Democrats in Congress to continue fighting for lower prescription drug prices and better access to affordable health care. Voters should reject the pernicious policies of Hershel Walker’s party, which seems to care more about their wealthy and powerful patrons than working people – and re-elect Senator Raphael Warnock.


