
The federal law providing seniors with nutritional services turns half a century old today. In 1972, the Congregate Meals program was added to the Older Americans Act (OAA) providing seniors in need with food in community settings. Six years later, Congress amended the OAA again to include home delivered meals for older Americans. Meals on Wheels is probably the best-known recipient of federal funding under this part of the law.
Though the nutrition provisions were added to the OAA during the Nixon administration, they represent a widening of President Lyndon Johnson’s original vision of a Great Society that takes care of its most vulnerable citizens, including and especially seniors. Nutrition was a natural bookend for a new era of health care for the elderly that began with Medicare, Medicaid, and the Older Americans Act – all of which were signed into law by President Johnson in 1965.
“A Great Society doesn’t let its most vulnerable citizens live in poverty or go hungry. Adding a nutrition program to LBJ’s vision of the Older Americans Act was a compassionate step to make the program more fully serve the needs of seniors.” – Dan Adcock, Director of Government Relations and Policy, National Committee to Preserve Social Security and Medicare
There are two types of nutrition programs under the Older Americans Act – congregate meals and home-delivered meals, both designed to supply lower-income seniors with hot, healthy food on a regular basis.
Congregate Meals
The Congregate Meals program encourages seniors to get out of the house, socialize with other people, and eat at least one nutritious meal a day in a community setting. Many congregate meal centers were forced to closed because of the pandemic. But they are slowly beginning to reopen.
Home-Delivered Meals often provide seniors who can’t easily leave their homes with nutrition and social contact they wouldn’t otherwise have. Since it wasn’t safe for many seniors to leave their homes during the pandemic, the need for home delivered meals became even more apparent. That’s why the home-delivered meals program needs to have the capacity to scale-up to handle future emergencies.
Social Interaction
Both nutrition programs present an opportunity for seniors who may otherwise be isolated to get some much-needed social interaction. Whether it’s a Meals on Wheels volunteer coming to the home and providing company or seniors sitting together enjoying a congregate meal, nutrition programs are a great antidote for lack of social stimulation.
Health Consequences
Seniors who eat regular, healthy meals are generally healthier than older people who don’t get proper nutrition. On the other hand, seniors face serious health consequences from not having proper access to nutritious meals – known as “food insecurity.”
“Malnutrition and unintentional weight loss contribute to progressive decline in health, reduced physical and cognitive functional status, increased utilization of health care services, premature institutionalization, and increased mortality.” – National Center for Biotechnology Information
More Work to Be Done
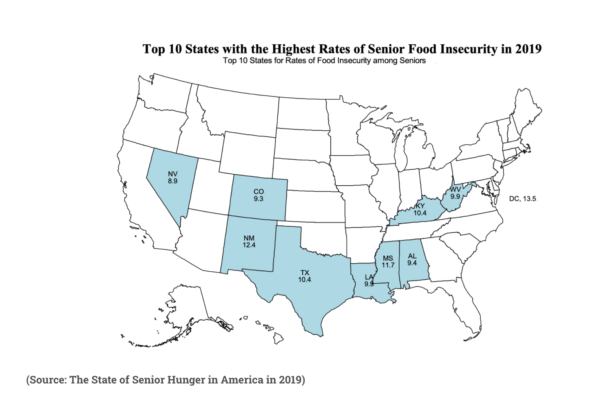
Despite fifty years of effort by governments and NGO’s, there is more work to be done in the area of senior nutrition. According to a 2019 study by Baylor University, 7% of Americans age 60 and over are food insecure, and 2.6% have very low food security. In fact, the number of seniors with very low food security has soared by over 200% since 2001. (The study was conducted before the pandemic, during which the numbers may have increased.)
Food insecurity among seniors, like many other metrics, is worse for the poor, racial minorities, younger seniors (60-69), and people who rent their homes.
 Over the past 20 years or so, funding for OAA nutrition programs failed to keep pace with the growth of the senior population and other demographic changes. (10,000 Americans turn 65 every day.) Eligible seniors have faced waiting periods for many OAA services, including home delivered meals, in most states.
Over the past 20 years or so, funding for OAA nutrition programs failed to keep pace with the growth of the senior population and other demographic changes. (10,000 Americans turn 65 every day.) Eligible seniors have faced waiting periods for many OAA services, including home delivered meals, in most states.
Fortunately, for Fiscal Year 2020, total OAA funding, including supplemental funding to respond to the needs of seniors during the COVID-19 pandemic, reached its highest level ($3.220 billion) in the Act’s five-decade history. This trend continued into Fiscal Year 2021 with an increase of $96 million. While it took a pandemic to finally provide adequate funding for the Older Americans Act, the National Committee and other seniors’ advocates hope that Congress will give senior nutrition programs the attention they need – and deserve.


